A Descent into Darkness
Unlike the more exotic diseases that capture the public’s imagination, Depression is a common, pervasive, and devastating condition that affects millions worldwide. Despite its ubiquity, it remains shrouded in misconceptions and stigma. I know this all too well because I have walked through its dark corridors, grappling with its crippling effects firsthand.
It began subtly, almost imperceptibly. At first, it was just a fleeting sadness, a temporary cloud that I believed would soon pass. But as the days turned into weeks, the cloud grew darker and more oppressive, overshadowing every aspect of my life. I found myself withdrawing from activities I once loved, unable to muster the energy or enthusiasm to engage with the world around me. It was as if a heavy weight had settled on my chest, making it difficult to breathe, to move, to live.
Depression is not just feeling sad or “down” after a disappointing event; it is a profound and persistent state of despair that can cripple an individual’s ability to function. I experienced this firsthand, as simple tasks became insurmountable challenges. The prospect of getting out of bed in the morning felt like a Herculean effort, and the idea of facing the world was overwhelming. I was trapped in a relentless cycle of hopelessness, unable to see a way out.
The Overwhelming Prevalence of Depression
My personal struggle is far from unique. Current estimates suggest that approximately 280 million people suffer from depression worldwide. According to the World Health Organization,
Mental disorders account for 1 in 6 years lived with disability. People with severe mental health conditions die 10 to 20 years earlier than the general population. And having a mental health condition increases the risk of suicide and experiencing human rights violations.
This alarming prevalence underscores the importance of understanding and addressing this mental health crisis.
The Symptoms and Severity of Depression
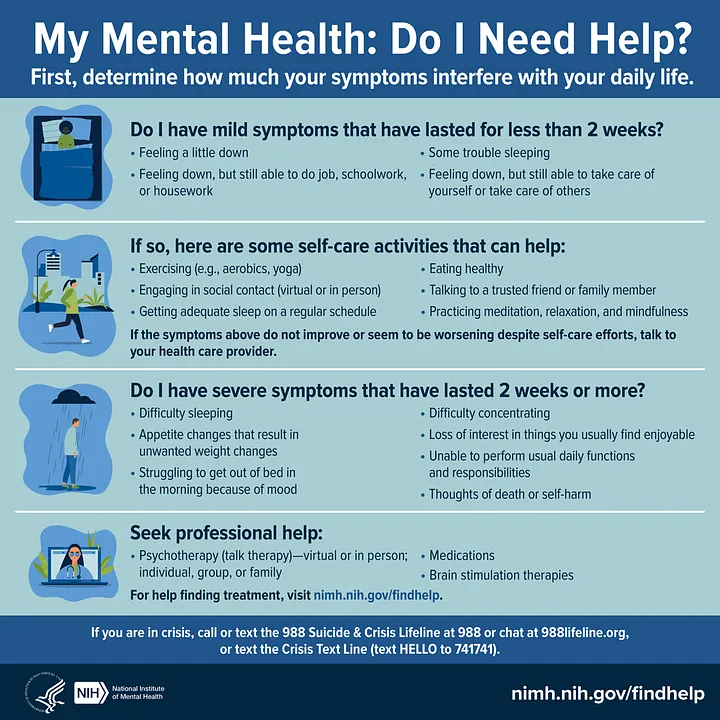
Depression manifests in various forms and severities, often classified into three primary categories:
- Everyday Depression: Temporary feelings of sadness or disappointment that everyone experiences from time to time.
- Reactive Depression: Significant but temporary depressive episodes triggered by major life events such as job loss, divorce, or the death of a loved one. These episodes typically resolve as the individual processes the event and begins to heal.
- Major Depression: A severe and enduring form of depression that persists for weeks, months, or even years, often without a clear external trigger. Individuals with major depression may experience recurrent episodes that become progressively detached from any specific cause.
I fell into the third category, where the despair was not linked to any specific event but was a constant, unrelenting presence. The most debilitating symptom for me was anhedonia, the inability to experience pleasure. Activities that once brought joy now felt hollow and meaningless. I remember standing on a beach, watching a beautiful sunset, and feeling nothing. It was as if the vibrant colors had been drained from the world, leaving only shades of gray.
The Biological Basis of Depression
Understanding the biological underpinnings of depression is crucial for developing effective treatments. Research has identified several key neurotransmitters and brain regions involved in depression:
- Neurotransmitters: Chemicals like norepinephrine, serotonin, and dopamine play significant roles in regulating mood. Imbalances in these neurotransmitters are linked to various symptoms of depression. For instance, reduced dopamine levels are associated with anhedonia, while serotonin deficiencies are linked to obsessive grief and guilt.
- Neuroanatomy: Brain imaging studies have revealed that individuals with depression often exhibit abnormalities in specific brain regions, such as the limbic system (involved in emotion) and the prefrontal cortex (involved in decision-making and self-regulation). These structural and functional changes contribute to the emotional and cognitive symptoms of depression.
- Hormonal Influences: Hormones such as cortisol (a stress hormone) and thyroid hormones can also impact depression. Elevated cortisol levels are common in individuals with depression, indicating a hyperactive stress response. Additionally, hormonal fluctuations related to reproductive events (e.g., postpartum depression, premenstrual dysphoric disorder) can increase the risk of depressive episodes in women.
The Psychological Dimensions of Depression
While biological factors are critical, the psychological aspects of depression cannot be overlooked. Freud’s distinction between mourning and melancholia provides a valuable framework for understanding depression. Mourning refers to the natural process of grieving a loss and eventually recovering. Melancholia, or major depression, involves a more complex and pathological response to loss, characterized by excessive self-criticism and internalized anger.
The concept of learned helplessness further elucidates the psychological mechanisms of depression. Individuals who repeatedly experience uncontrollable stressors may develop a sense of helplessness and hopelessness, believing they have no control over their circumstances. This cognitive distortion can perpetuate and exacerbate depressive symptoms.
Biology and Psychology
Depression arises from a webbed relationship of biological, psychological, and environmental factors. Stress, particularly during critical developmental periods, can predispose individuals to depression by altering brain chemistry and function. For instance, children who experience significant stressors, such as parental loss, are more vulnerable to depression later in life.
Recent research has identified specific genes that interact with environmental stressors to increase the risk of depression. For example, certain variants of the serotonin transporter gene can heighten susceptibility to depression following stressful life events. This gene-environment interaction underscores the importance of considering both biological predispositions and life experiences in understanding depression.
The Maze of Treatment
Although it may oftentimes feel tedious to talk about the treatments of these things, as this isn’t supposed to be some academic discourse. It is a crucial thing to talk about, over and over again, so that our brains envelope this as a mantra of sorts for whenever in life we may need it. Effective treatment of mental disorders often requires a multifaceted approach that addresses both biological and psychological factors:
- Medications: Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants have helped correct neurotransmitter imbalances. *Do not self-medicate!*
- Psychotherapy: Cognitive-behavioral therapy (CBT) and other forms of talk therapy have been invaluable in identifying and changing negative thought patterns, and developing healthier coping strategies. *No one to talk to? Write a blog!*
- Lifestyle Changes: Regular exercise, a balanced diet, and adequate sleep have supported my overall mental health and alleviated some depressive symptoms. *Delete all those sad songs you love so much, and embrace sunshine and rainbows!*
- Social Support: Building strong social connections and seeking support from friends, family, or support groups has provided emotional relief and practical assistance. *This one’s going to be especially alot of work*
The Importance of Awareness and Compassion
Despite the biological and psychological realities of depression, stigma and misunderstanding persist. Depression is often mistakenly seen as a sign of weakness or a failure to “pull oneself together.” This stigma can prevent individuals from seeking help and exacerbate their suffering.
It is crucial to recognize depression as a legitimate and serious medical condition that requires understanding, compassion, and appropriate treatment. Just as we would not blame someone for having diabetes (or not producing enough insulin!), we should not blame individuals for experiencing depression (or not producing enough serotonin!).
It is my hope that these words resonate with the world to foster a more empathetic and informed society. So that we can support those affected by depression and promote mental health for all.
A Call to Action
Depression is a pervasive and crippling disorder that affects millions of people worldwide. Its complexity requires a comprehensive approach that integrates biological, psychological, and social perspectives. By advancing our understanding of depression and addressing it with compassion and effective treatments, we can alleviate the suffering of those affected and improve the overall well-being of our society.
In a community that values high achievement and excellence, such as a university setting, acknowledging the prevalence and impact of depression is particularly important. Creating an environment where individuals feel safe to seek help and discuss their mental health openly can lead to better outcomes and a healthier, more supportive community.
As someone who has walked this path, I can attest to the transformative power of understanding, empathy, and appropriate care in traversing the depths of depression.
Help raise awareness about depression, which is one of the most common mental disorders in the world, by sharing informational materials based on the latest research. Share science. Share hope. https://go.nih.gov/anhTIQn